Silica Exposure Statistics: What Workers & Advocates Should Know
Silica exposure remains one of the most persistent and preventable occupational health risks in the United States. Millions of workers breathe air containing tiny crystalline silica particles that can scar lung tissue and cause serious diseases such as silicosis, chronic obstructive pulmonary disease, and lung cancer. This page explains what silica is, how exposure occurs, who is most at risk, and what workers and advocates should know about prevention, and regulations.
Home » Silica Exposure Statistics: What Workers & Advocates Should Know
What Is Silica?
Silica, scientifically known as silicon dioxide, is a naturally occurring mineral composed of silicon and oxygen. It is one of the most abundant substances on Earth, found in sand, rock, soil, clay, and many construction and manufacturing materials. According to the National Center for Biotechnology Information and the Agency for Toxic Substances and Disease Registry, there are two major forms of silica: crystalline and amorphous. Both share the same chemical composition but differ in internal structure, which affects how they behave in the environment and the human body.
Amorphous Silica vs. Crystalline Silica
Amorphous silica, or a-silica, lacks a fixed crystal structure; its atoms are randomly arranged. It is often found in glass, diatomaceous earth, and synthetic materials such as silica gels and fumed silica. By contrast, crystalline silica, or c-silica, has an ordered, repeating pattern of silicon and oxygen atoms. Quartz is the most common crystalline form, although others, like cristobalite and tridymite, also exist.
Both types can interact with human lung cells, but research shows crystalline silica produces a much stronger and longer-lasting inflammatory response. Studies on crystalline and amorphous silica found that while both stimulate lung fibroblasts, crystalline silica induces more persistent activation, increasing the risk of fibrosis and silicosis. Respirable crystalline silica, or RCS, particles are extremely small—at least 100 times finer than the sand found on beaches. This allows them to penetrate deep into the lungs, where they can cause irreversible scarring.
Amorphous Silica
Crystalline Silica
What Is Silica Exposure and Why Does It Matter?
Silica exposure occurs when people inhale respirable crystalline silica dust generated by cutting, drilling, grinding, or otherwise disturbing materials that contain silica. While silica exists naturally in the environment, the particles most dangerous to health are those small enough to reach the deepest parts of the lungs.
Awareness about silica exposure matters because it is so widespread yet largely preventable. Everyday materials such as concrete, asphalt, brick, stone, and glass release hazardous dust during industrial work. Prolonged or repeated inhalation can cause silicosis, an incurable lung disease, and increase the risk of lung cancer, kidney disease, and autoimmune disorders. Even short-term exposure to extremely high concentrations can trigger acute silicosis, a rapidly fatal form of lung damage.
Key Statistics on Silica Exposure and Facts
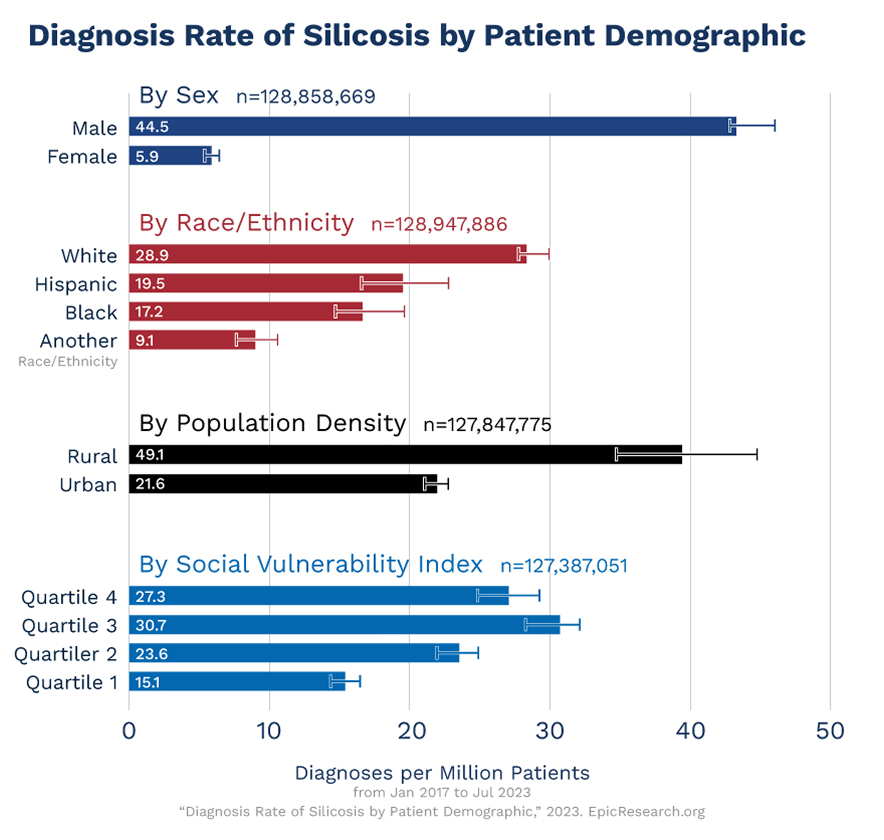
Silica exposure remains a major public health and workplace safety issue. While national rates of silicosis have declined gradually, new clusters of cases, particularly in engineered stone fabrication and mining, indicate that the problem persists.
The following statistics highlight the current scope of silica exposure and its impact on American workers:
- Approximately 2.3 million U.S. workers are exposed to silica on the job, including roughly 2 million in construction and 300,000 in other industries.
- OSHA’s Permissible Exposure Limit, or PEL, for respirable crystalline silica is 50 micrograms per cubic meter of air, or µg/m³, averaged over an 8-hour shift.
- The National Institute for Occupational Safety and Health, or NIOSH, recommends an even stricter Recommended Exposure Limit, or REL, of 50 µg/m³ over a 10-hour workday.
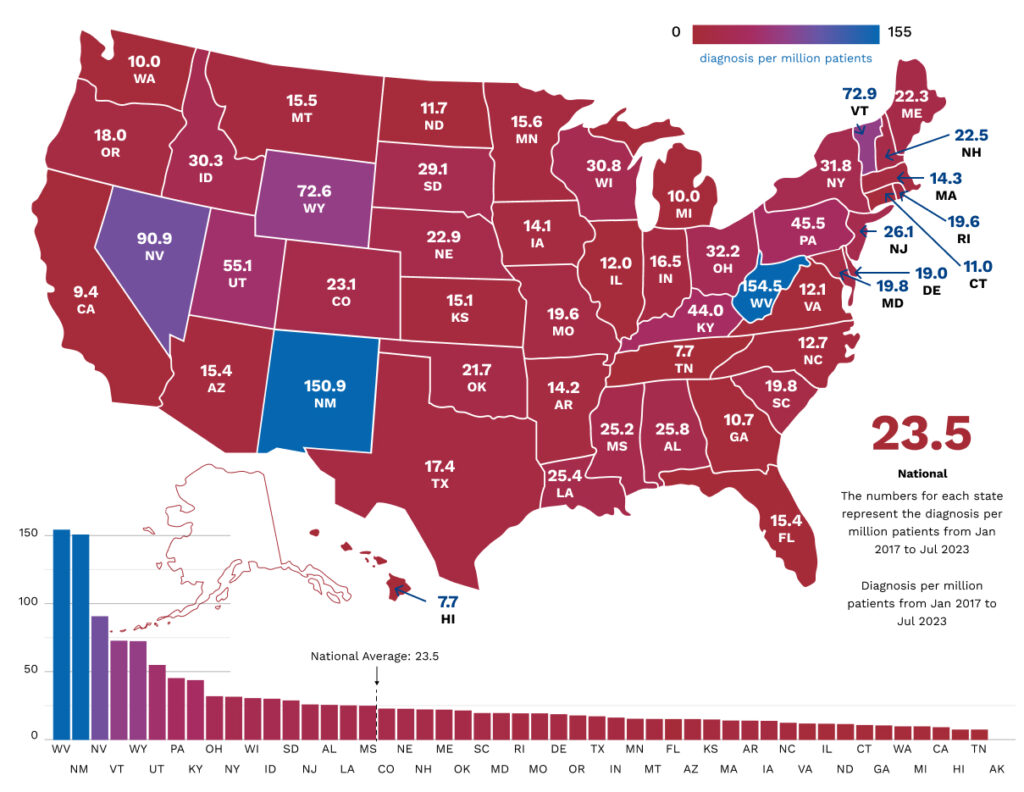
- The rate of silicosis diagnoses has declined nationwide, from 8 per million in 2017 to 6 per million in 2023. However, cases continue to emerge in high-risk states like West Virginia, New Mexico, and Nevada.
- Complications from silicosis can include tuberculosis, lung cancer, chronic bronchitis, autoimmune disorders, and kidney disease.
- There is no cure for silicosis. However, treatment and preventive measures can help you avoid the disease entirely or slow its progression.
Which Occupations Are Most at Risk for Silica Exposure?
Silica exposure primarily affects industries that disturb rock, soil, or mineral-based materials. Workers in these environments generate or encounter airborne dust by cutting, grinding, drilling, or crushing silica-containing substances. According to OSHA and NIOSH, the highest-risk sectors include construction, mining, foundry work, oil and gas extraction, and ceramics manufacturing.
How Are Artificial Stone Fabricators Exposed to Respirable Crystalline Silica Dust?
- Engineered stone used for countertops contains over 90% crystalline silica, which is significantly higher than in granite (40–50%) or marble (<10%).
- OSHA inspections in 2022 found that about 25% of breathing zone samples from fabrication shops exceeded the silica exposure limit, with some readings reaching 20 times the PEL.
- Cases of accelerated silicosis have been reported in young workers with severe disease developing within 7–19 years of exposure.
During dry processing, workers who cut, grind, or polish engineered stone can inhale fine silica dust that becomes airborne. Despite the use of wet cutting and ventilation systems, studies have shown that respirable silica concentrations often exceed safe levels. Many fabrication shops lack written exposure control plans or respiratory protection programs.
Recent OSHA enforcement data highlight the human cost: multiple workers in California’s countertop industry developed silicosis so severe that several required lung transplants, and some died in their 40s. This underscores the urgent need for stronger protective regulations in the United States.
How Are Construction Workers Exposed to RCS?
- About 2 million construction workers are exposed to respirable crystalline silica across 600,000 worksites nationwide.
- Common exposure activities include sandblasting, drilling, concrete cutting, sawing, grinding, and jackhammering.
- OSHA’s silica standard requires employers to limit exposure to 50 µg/m³ and follow certain control methods.
Construction tasks often generate dust clouds from materials like brick, concrete, and stone. The most severe exposures occur during sandblasting and surface preparation of bridges, tanks, or buildings. Without engineering controls, workers can inhale dangerous levels of silica.
OSHA calls for safe practices, including using saws equipped with integrated water delivery systems, HEPA-filtered vacuums, and protective respirators when needed. Employers must also train workers, conduct exposure assessments, and maintain written control plans. Despite these regulations, many construction sites continue to report overexposure, underscoring the need for consistent enforcement and education.
How Are Miners Exposed to Silica Dust?
- Between 2000 and 2019, over 55,000 silica samples were collected from U.S. mines.
- 11.8% exceeded OSHA’s PEL, and 27.3% exceeded NIOSH’s REL.
- Surface mines accounted for nearly 87% of samples, but exposure levels were similar in underground operations.
- Increased r-type opacities on X-rays suggest higher silica exposure among coal miners, particularly in Central Appalachia.
Silica dust in mining originates from drilling, blasting, cutting, or transporting rock. Surface and underground miners inhale crystalline particles released from quartz-rich materials. The Mine Safety and Health Administration, or MSHA, studies show chronic overexposure in multiple mining sectors. In coal mines, the resurgence of severe pneumoconiosis in Appalachian regions is linked to high silica concentrations in dust generated by thinner coal seams.
Even with advances in dust control and monitoring, miners continue to face substantial risks, emphasizing the need for stricter exposure assessments and enforcement under MSHA’s new silica rule.
How Are Foundry Workers and Metal Casters Exposed to Silica?
- Foundry work involves handling sand molds, which are composed largely of silica.
- Studies show 9.6% of foundry workers and 2.9% of automotive foundry employees exhibit signs of silicosis.
- Tasks like sand handling, shakeout, grinding, and abrasive cleaning generate respirable dust.
Silica exposure in foundries occurs when sand cores and molds are made, broken apart, or cleaned. High-temperature processes can release fine silica particles into the air. Inadequate ventilation and insufficient personal protective equipment amplify the danger. NIOSH emphasizes that comprehensive ventilation systems, enclosed shakeout areas, and regular medical surveillance are critical to reducing silica exposure in foundries and preventing silicosis among metal workers.
How Are Oil and Gas Extraction Workers Exposed to RCS Dust?
- Hydraulic fracturing, or fracking, operations utilize large volumes of quartz sand that contains crystalline silica.
- NIOSH identified seven major dust sources during fracking, including sand transfer belts, blender hoppers, and sand movers.
- Exposure monitoring has revealed airborne silica concentrations up to 10 times the recommended limit.
When sand is moved, mixed, or poured into hydraulic fracturing equipment, silica dust becomes airborne. Workers at sand movers, blender hoppers, and truck filling stations are especially at risk. Despite the use of enclosed cabs and ventilation systems, NIOSH sampling across multiple sites reveals that exposure levels frequently exceed the REL. Control measures are critical to preventing disease. Such measures include reducing sand drop distances, installing exhaust ventilation, and providing respirators.
How Are Ceramics Manufacturing Workers Exposed to Silica Dust?
- The ceramics and pottery industries utilize silica-rich materials, including clay and glaze.
- Epidemiological studies show an increased risk of kidney disease and lung disorders among ceramic workers.
- Observed disease rates were over three times higher than expected, particularly among workers employed for fewer than 20 years.
Tasks such as mixing clay, molding, firing, and grinding produce respirable silica dust. Studies have shown elevated risk even in non-smokers, suggesting that silica exposure alone drives much of the disease burden. Workers without visible silicosis also exhibited renal effects associated with long-term silica exposure. Proper enclosure of mixing operations, utilizing wet processes, and the use of respiratory protection are essential in ceramics manufacturing to minimize airborne dust.
What Are the Health Risks of Silica Exposure?
Understanding the medical consequences of silica exposure is critical for early detection, proper diagnosis, and legal accountability. The most well-known illness linked to silica dust exposure is silicosis, an incurable occupational lung disease that progresses even after exposure stops. Silicosis appears in three main forms:
- Chronic silicosis usually develops after 10 to 30 years of low-level exposure and may remain unnoticed for years before symptoms such as shortness of breath and fatigue appear.
- Accelerated silicosis typically develops within 5 to 10 years of higher exposure, often in industrial settings where dust control measures are inadequate.
- Acute silicosis can develop within months following extremely high exposure to silica dust, leading to rapid and severe respiratory failure.
In all forms, silicosis causes inflammation, scarring known as fibrosis, and the gradual destruction of lung tissue. Symptoms may include shortness of breath, chest pain, coughing, fever, and fatigue. As the condition advances, patients may struggle with even light activity or require long-term oxygen therapy. Silica exposure is also associated with several other serious health conditions:
- Lung cancer: The U.S. Department of Health and Human Services and the International Agency for Research on Cancer, or IARC, classify crystalline silica as a known human carcinogen. Long-term exposure substantially increases the risk of developing lung cancer, particularly for workers in mining, construction, and stone fabrication.
- Chronic Obstructive Pulmonary Disease, or COPD: Repeated or prolonged exposure can cause chronic bronchitis and emphysema, leading to irreversible airway obstruction and diminished lung capacity.
- Kidney disease and autoimmune disorders: Studies have linked long-term silica exposure to kidney damage and autoimmune conditions such as lupus, scleroderma, and rheumatoid arthritis, suggesting that silica may trigger immune system dysregulation.
Cigarette smoking further compounds these risks, accelerating the decline of lung function and increasing susceptibility to cancer and respiratory failure. For workers exposed to silica dust, avoiding tobacco use and participating in regular medical surveillance are critical steps in preserving health and detecting disease early.
How Can Workers Prevent or Reduce Silica Exposure?
OSHA and NIOSH recommend using a layered approach, combining engineering controls, safe work practices, personal protective equipment, and regular monitoring, to minimize silica dust exposure. Together, these strategies form the foundation for a compliant and effective silica exposure control program.
Engineering Controls: Use wet cutting, drilling, or grinding methods and install local exhaust ventilation to capture dust at its source. Shrouded tools connected to HEPA-filtered vacuums further reduce airborne silica.
Safe Work Practices: Avoid dry sweeping or using compressed air. Instead, clean with wet sweeping or HEPA vacuums, maintain dust-control systems, and replace filters and water regularly to prevent recirculation.
Personal Protective Equipment: When dust levels cannot be reduced below limits, provide NIOSH-approved respirators. Ensure that fit testing, training, and medical clearance are implemented for all respirator users.
Air Monitoring and Compliance: Conduct routine air sampling using NIOSH Methods to measure silica concentrations. Maintain exposure records and take corrective action if levels exceed OSHA’s PEL.
Written Exposure Control Plans: Identify tasks that create silica dust, assign a person to oversee compliance, restrict access to high-exposure areas, and provide regular employee training.
Medical Surveillance and Education: Offer exposed workers periodic chest X-rays and lung function tests to monitor their health. Educate employees about the symptoms of silicosis and the importance of seeking early medical evaluation.
Culture of Prevention: Encourage workers to report unsafe conditions and ensure that timely corrective action is taken. Reinforcing that prevention, not treatment, is the only true defense against silicosis and other silica-related diseases.
OSHA and NIOSH jointly oversee exposure assessment protocols and a National Emphasis Program to standardize compliance across high-risk industries. This coordinated effort ensures that both employers and workers have clear, enforceable protections that keep pace with evolving workplace hazards.
While significant progress has been made in controlling exposure, continued vigilance, enhanced safety protocols, and comprehensive worker education remain critical to reducing the risk of silica-related diseases. With ongoing efforts to adapt to new challenges, we can protect workers and create safer, healthier workplaces for the future.
